
I am currently implementing the Dynamic Patient Positioning Protocol – Sensory Assisted Application (DPPP-SAA), as the main treatment protocol in my spine clinic. This is a specific and unique treatment procedure which I have personally designed and improved throughout my 33 years of clinical experience. This protocol is based upon Flexion / Distraction technique, applicable to variety of spinal column Inter-Segmental Dysfunctions (ISD), discopathies, as well as structural and functional spinal deformities.
The DPPP-SAA is a protocol that allows for specific individualized treatment procedure based on patient’s presentation. It is important to note that even so there are similarities in patient treatment procedures, yet in this particular system, the treatment protocol is tailored specifically for each individual patient. Subsequently, in addition to standard examination procedures and advanced imaging study results, it is the bio-mechanical diagnosis that is also taken into consideration, allowing for a more accurate selection of the appropriate treatment procedure.

More specifically, even the morphology of the affected inter-vertebral disc itself is considered a consequential component in this selection. It is important to emphasize that with this system, treatment procedure of a far lateral disc herniation for example, is rather different from the treatment procedure of a posterio-lateral herniation, or even a hyper bulged disc.
Consequently, it is the specificity of the treatment protocol that allows for a safer more effective treatment, which has also significantly improved the long-term prognosis. In fact, during treatment of complicated cases with advance structural pathology, serial MRI studies within the first 4-6 weeks, 12 weeks, and 24 weeks follow-up study may be necessary to monitor structural improvement and the long term prognosis.
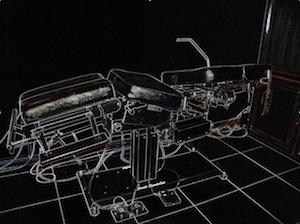
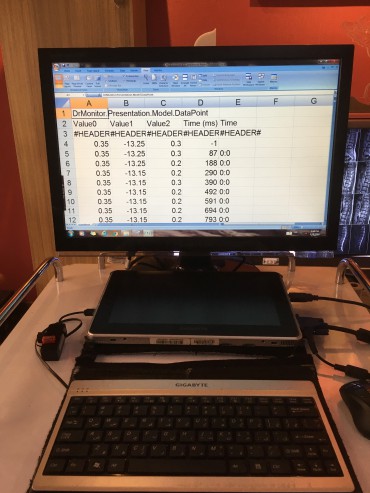
The Sensory Assisted Application is supported by the S1-Active Locus Monitoring Instrument hardware. This instrument which I have also designed and patented, not only allows for live monitoring of the specific treatment procedure, but it is also capable of recording the precise detail of each treatment session. As the result, the accumulated data has proven to be highly valuable for the study of different treatment procedure results and their clinical efficacy. Furthermore, specific treatment procedures for patients with similar clinical – neurological presentations, can be objectively categorized for the purpose of clinical correlation, post-doctorate education, and related research projects.
As a basic principle, patients with localized, or even radicular pain are expected to respond well to the DPPP-SAA treatment protocol within the first few sessions. Response to treatment is measured by meaningful reduction in chief complaint, improved neurological presentation, and appropriate functional improvement detected by the S1-Active Locus Monitoring Instrument.

It is important to emphasis that proper patient selection is just as essential as the treatment protocol itself. Generally speaking, patients with stable ISDs and discopathy without a progressive neurological deficit can be considered potential candidates for this treatment protocol. In fact, bio-mechanical stability does not necessarily correspond to the severity of structural pathology seen on the imaging study. Case in point, a large herniation or even a focal extrusion may be more stable from the bio-mechanical perspective, than a degenerated-desiccated hyper-bulged disc.
Therefore, a high-quality MRI imaging study, which in some cases must also be complimented by stress or bone window studies, is necessary for establishing an accurate bio-mechanical diagnosis, and subsequent correlation with clinical – neurological findings.
It is also important to recognize that DPPP-SAA treatment protocol is applied along the axial plane with a well controlled decompression components, and a minimal lateral or axial rotation. It is therefore considered a safe procedure, even in cases of a more advanced discopathies and their related clinical – neurological presentations.
Please note that some of the pre-treatment and post-treatment comparison results can be viewed in the Case Studies section of this website.
Hossein Sabbagh, D.C.
Published: November 08, 2019
Updated: September 27, 2021