Narrative
One of the acceptable approaches to conservative treatment of spinal bio-mechanical disorders is the use of Automated Supine Decompression systems being advocated by some companies and clinicians in their respected fields. Even so I personally do not use this system, however, I have seen positive treatment results on selected patients.
This particular case report involved a 46 years old white male who had presented to a clinician (specializing in a different health discipline) with a chief compliant of subacute mild – moderate left L4-5 radiculitis extending to the lower back and the left gluteal region, of two weeks duration. He had denied any specific cause including trauma, and reported an insidious onset. He did indicate having had experienced a self limited mild, occasional low back pain in the past (based on obtained patient files).
At the time of his initial examination and according to the patient’s file, there was some limitation of right lateral flexion (L/S). SLR was positive on the left at 55 degrees with limited radiation to the posterior knee, and muscle testing was 5/5 with intact DTR.
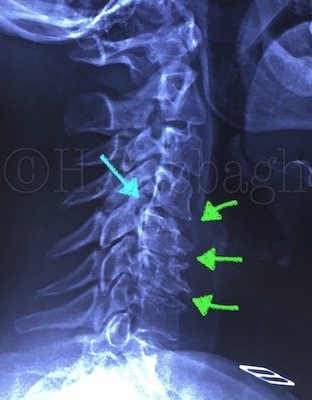
The initial MRI study obtained just prior to the initiation of treatment indicated L4-5 posterior lateral left herniation, extending into the sub-articular space, corresponding to the initial clinical presentation (Plates: 1-2/8).
Case Report – 32 [Pre-treatment MRI Study Plates (1/8)]
Following the initial examination, patient was treated for total of ten sessions, which had included the use of physical modalities, with the Automated Supine Decompression unit as the main protocol. No form of manipulation including osteopathic or long lever type was applied in this case.
According to the treating clinician, and later confirmed by the patient, he did not report any significant discomfort during the treatment sessions. However, he had reported change in his pain pattern following the fourth session of treatment.
The treating clinician had also performed a re-evaluation following the sixth session of treatment, with apparently “fair” results.

Case Report – 32 [Pre-treatment MRI Study Plates (2/8)]
Following the tenth session of treatment, patient was prescribed an exercise program, first two sessions of which was performed under supervision of a qualified physiotherapist, with further instructions on hydro-therapy. This patient was also scheduled for a re-examination within two weeks following the last session of supervised exercises.
According to the patient following his initial release from care, he had noticed further changes in his pain pattern. More specifically the lower back and left gluteal pain had improved, yet he was experiencing progressive left lower extremity pain, extending into the left ankle.
He also reported eventual onset of paresthesia of the left lateral leg and the dorsal area of the left foot, which were not previously present. This was in addition to having experienced discomfort during some of the stretching exercises which were becoming progressively more painful.
Patient also strongly denied any other possible exacerbating event, and he insists that he had abided by the given instructions, and had in-fact rested at home for the period of one week following his last treatment session.
Regardless of his conflicting pain pattern, he did wait for two weeks, as scheduled, before reporting back to the treating clinician, whom upon re-examination found rather unexpected re-evaluation results.
At that time, this patient was referred to my office for further consultation by a fellow clinician at the same center, who had also examined the patient.
Unfortunately, I was unable to examine this patient until 6 weeks following his referral. He had however, consulted a pain specialist during this period, and had received further treatment including low back corticosteroid injection, followed by anti-inflammatory medication, and recommendation of two weeks of complete rest, which were beneficial.
Despite all the aforementioned efforts, and at the time of his initial examination at my office, patient appeared tense, and in significant pain. In fact he was unable to sit comfortably for even a few minutes, and preferred to stand up. Examination also revealed significant antalgic lean, difficulty with left heel walk, reduced left knee DTR, hypotonicity of the left lower extremity particularly the left tibialis anterior and the extensor hallucis longs were 3/5. SLR was positive at 20 degrees, and CSLR at 40 degrees.
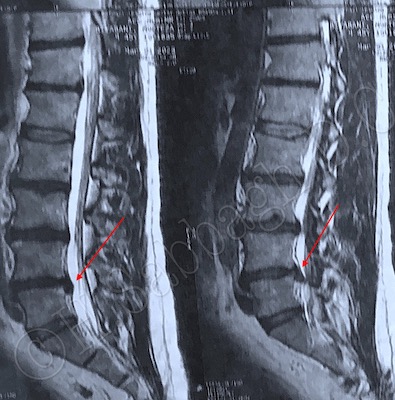
Subsequently I ordered a follow up MRI study (which was obtained 9 weeks following the initial study) result of which can be seen on the plates 3-4/8.

Case Report – 32 [Post-treatment MRI Study Plates (3/8)] 
Case Report – 32 [Post-treatment MRI Study Plates (4/8)]
The follow up MRI study clearly indicated significant expansion of the herniated material involving the sub-articular space (Red Arrows), as well as compromising the left lateral recess at L4-5 segment.
Following clinical correlation with the diagnostic imaging findings, I referred the patient to a neurosurgeon for surgical intervention with priority.
The purpose of this case report presentation is not to question an specific treatment protocol such as the Automated Supine Decompression system which was used in this particular case, but to review the clinical decision making process, through out the treatment procedure and the follow up.
More importantly, pointing out the importance of abiding by the Clinical Practice Guidelines set forth, in order to prevent possible complications such as this particular case, or similar cases which may lead to unfavorable treatment outcomes.