Discussion
The purpose of this case report is to review the clinical decision making process which was implemented in both examination, working diagnosis, as well as implementation of the treatment protocol in this particular case.
Even so I personally do not use automated decompression systems (supine or otherwise), yet this is an acceptable procedure being used successfully by some clinicians, including some Doctors of chiropractic.
Lets review some of the clinical decision makings processes applied in treatment of this particular patient, and correlate them with the current Clinical Practice Guidelines set forth by the Commission on Chiropractic Clinical Practice Guidelines (CCCPG) (IRCA):

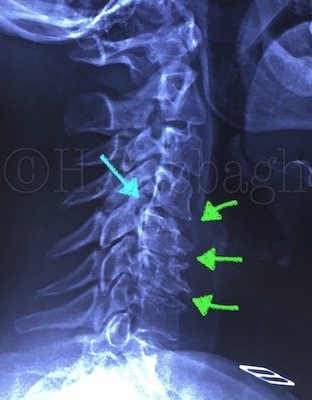
Case Report – 32 [Pre-treatment MRI Study Plates (5/8)]
1. The initial advanced diagnostic imaging (MRI) study indicates L4-5 posterior lateral left, limited herniation with extension into the sub-articular space, but short of the lateral recess. It did in fact correspond to the initial chief compliant’, and patient’s clinical presentation. However; inadequate attention was paid to the presence of Modic Type II changes seen at the posterior 1/3 f the L5 Superior end plate, and L4 inferior end plate (Plates: 5-6/8 Red Arrows).
Even so Modic type II changes may indicate relative stability (in comparison to modic type I), yet it can suggest chronic degenerative changes, with resultant instability. In this particular case, further instability of the posterior compartment is suggested.
This finding did correlate with patient reporting occasional lower back pain in the past. Recognition of this specific imaging finding should have triggered the treating clinician to consider the possibility of an unstable L4-5, being further complicated by the recent discopathy, and possible hypo-mobility of the L5-S1 segment (Plate: 6/8 Blue Arrow).
This observation alone warranted obtaining a stress study in order to further evaluate the extent of instability, and furthermore; modify the automated supine decompression procedure accordingly. If the Automatic Supine Decompression system is not specific enough (according to the treating clinician), then perhaps it was not suitable for treatment of this particular patient.

Case Report – 32 [Pre-treatment MRI Study Plates (6/8)]
2. Patient tolerance during decompression procedure may not be a reliable indicator of the extent nor the angle of decompression being applied. It is empirical to keep in mind that in cases of herniations with outer annular disruption, the leakage of the disc material may be gradual, explaining the eventual pain pattern from a lower back with radiculitis, to a severe radiculopathy through a course of several days, or in some cases a few weeks. Even in use of the Flexion / Distraction instrument, patient tolerance should not be used as the only clinical indication for the level or extent of decompression. Furthermore; every single discopathy may be present with a unique characteristics, as such, treatment procedure must be adjusted accordingly. If the utilized instrument lacks the necessary specificity, it should not be applied in complicated cases.
3. Based on the current Clinical Practice Guidelines, the initial re-evaluation is clearly indicated following the third treatment session. In some cases, this evaluation may be delayed for up to 48 hours for a better objectivity, but no other treatment in between is indicated including exercise programs.
Re-evaluation must include complete neurological work up as pertaining to the case in hand, functional re-evaluation including orthopedic examinations, and clear improvement in patients chief complaint based on 0-10 scale. Positive correlation of the above is mandatory for continuation of the treatment procedure. In this case however; re-evaluation was performed following the sixth session of treatment with little improvement in the chief complaint, and lack of detailed ortho-neuro re-evaluation results (according to patient’s file). At this stage the treatment procedure should have been stoped, in favor of further re-evaluation and possible referral.
4. According to the treating clinician and later confirmed by the patient, changes in the pain pattern was reported by the patient following the fourth session of treatment. Pain pattern changes are a common findings during decompression procedure, however; specific characteristics of these changes must be evaluated as it may indicate actual regression, oppose to improvement.
For example patient reported having reduced low back and left gluteal pain, conversely, he had also reported increased radicular pain. In other words the pain pattern was becoming more distal, as well as radicular, oppose to the proximization which should have been accomplished. Furthermore; addition of dermatomal paresthesia which did not exist before, should have been construed as a warning sign.
5. Every patient following the last continue treatment session must undergo another comprehensive re-evaluation, as described earlier, which was not performed in this case.
6. Prescribing exercise programs should only follow the pre-release clinical re-evaluation with objective documentation of neurological and functional improvement and more importantly stabilization, in addition to improvement of the chief complaint.
Generally speaking, stretching exercise must be prescribed cautiously in patients with discogenic pain, particularly with radicular involvement of any degree, even in stable cases.
7. Patient should have been advised to report back immediately to the treating clinician in case of any changes in his pain pattern, difficulty performing the prescribed exercise program, or initiation of any new symptoms particularly increased leg pain, and / or numbness and tingling, instead of waiting for the pre-scheduled re-valuation appointment.
8. Following the pre-scheduled re-evaluation results, a follow up MRI study should have been immediately obtained, and patient should have been referred directly to a neurosurgeon, saving a 6 weeks of waiting period.
9. The follow up MRI study obtained 9 weeks from the initial study, not only clearly indicates significant increase in herniated material, but it also further emphasizes posterior compartment instability at the involved segment (Plates: 7-8/8).

Case Report – 32 [Post-treatment MRI Study Plates (7/8)] 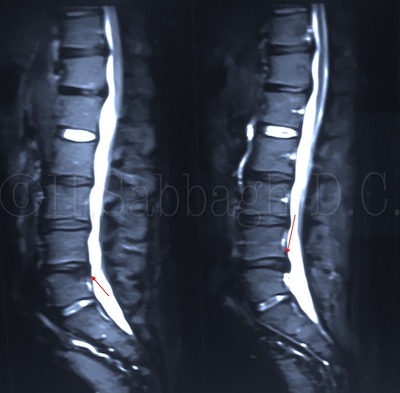
Case Report – 32 [Post-treatment MRI Study Plates (8/8)]
The Commission on Chiropractic Clinical Practice Guidelines (CCCPG) (IRCA) main purpose is to help establish clear guidelines on safe, effective, evidence based conservative treatment protocols, for Doctors of Chiropractic.
Even so this particular patient was treated by a fellow clinician of a different health discipline, yet sharing similar cases such as this can serve as a valuable learning tool for all of us involved in clinical management of patients with bio-mechanical disorders, particularly discopathy related conditions, which are rather a common findings in our health care system.
H. Sabbagh, D.C.
Published: June 24, 2023
©2023 H. Sabbagh D.C. (All Rights Reserved)