Narrative
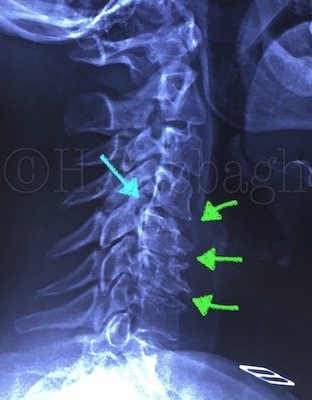
This is a 33-year-old patient who presented with a history of episodic lower back pain during the past several years. The area of chief complaint was limited to the lower back, and usually self-limited.
A few weeks ago and following a falling accident, the patient developed severe lower back pain, which within a few days extended into the lower left extremity.
Despite referring to a physician and receiving analgesics and anti-inflammatory medication, and two weeks of bed rest, the patient’s condition eventually regressed with numbness and paresthesia extending into the left leg.
At this stage, the patient referred to a pain specialist who recommended corticosteroid injections in the lower back followed by more than 30 sessions of physiotherapy. The initial PT therapy helped to reduce lower back pain. However, the final three sessions of PT included supine distraction via a decompression unit, following which the patient reported exacerbation of the left lower extremity pain, leading to discontinuation of the treatment program.
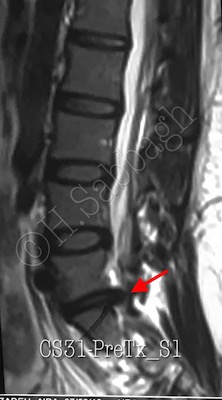
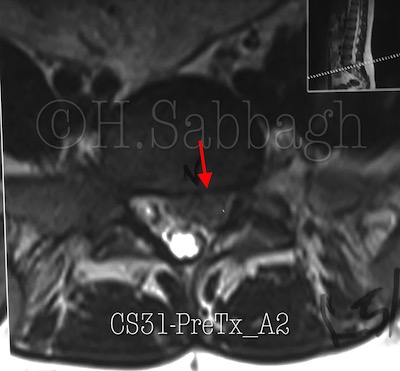
The patient was subsequently referred to a neurosurgeon, an MRI study was obtained (plates 1-4/8), and surgical intervention was contemplated.
This patient was admitted to my office a few days later, with clinical presentation of moderate to severe left S1 radiculopathy, reduced left ankle DTR, and a positive left SLR at 35 degrees, in addition to right SLR at 55 degrees. Muscle strength was intact, and the lumbo-sacral ROM altered in flexion & left lateral flexion..
Because of time delay in initiating the treatment protocol, the prognosis was guarded. Re-evaluation was scheduled following the third session of treatment via DPPP-SAA protocol.
Patient response to the initial treatment was significantly better than expected. It was therefore decided to continue the conservative treatment.
This patient reported about 40% reduction in the left lower extremity pain within the first five sessions of treatment confirmed by improved neurological and functional presentation.